Sign up to our newsletter Subscribe
Analysing Global Immunisation Expenditure

‘Choose something common and you will find little is known about it’ (Henry Head to the young Dr Russell Brain c 1920). Although common (8 per cent of the population) and recognised for more than 2,000 years, migraine has rarely commanded significant professional…
‘Choose something common and you will find little is known about it’ (Henry Head to the young Dr Russell Brain c 1920). Although common (8 per cent of the population) and recognised for more than 2,000 years, migraine has rarely commanded significant professional or public attention. It does not shorten life or cause permanent injury. In contrast to many current health problems examined in the Office of Health Economics’ series, the morbidity generated by migraine does not give rise to substantial costs borne by the National Health Service.
The ‘low profile’ image of migraine has also been fostered by several other factors. From a scientific perspective, although investigative techniques have advanced there have been no significant breakthroughs in understanding the aetiology of the disorder. Many theories about causation have been put forward but none proven: hypotheses include, inter alia, vasospasm, alterations in the metabolism of the neurotransmitter serotonin, food allergy, abnormalities of the blood-brain barrier, platelets and cerebral hypoxia. The debate over whether migraine is the result of disturbances in the vascular or neurological systems, started in the late 19th century, remains unresolved.
Various popular beliefs have grown up around migraine, for example, that it is a neurotic disorder, which, rather than generating positive concern, have tended to diminish sympathy that might otherwise have been extended to sufferers of the condition. A typical sufferer is popularly thought to be extremely intelligent, highly strung and a perfectionist. It is also perceived by some to be a hysterical female disorder. And others have used the term inappropriately to describe much more minor head pains as a means of giving greater justification to a decision not to do something, such as attend work.
Yet migraine is a much more significant disorder than might be suggested by these erroneous notions. In the first instance, migraine is experienced by a large number of people. Despite the availability of data from the many surveys that have been carried out, precise estimates of prevalence are difficult to obtain because of differing criteria to define cases of the disorder and variations in the proportion of cases likely to become known to the inquiring agency. Nevertheless, if estimates suggesting prevalence rates of between 7 and 10 per cent are correct, then there are currently 3.9 to 5.6 million migraine sufferers in the United Kingdom. This implies that migraine affects twice as many individuals as, for example, asthma, a disease that has featured much more prominently and regularly in both the medical and lay media.
Although migraine does not give rise to substantial financial costs to the National Health Service, the disorder can impose severe burdens on sufferers themselves. The impact of disease on quality of life and the effectiveness of medical interventions in improving the well-being of sufferers are topics that are increasingly attracting the attention of individuals responsible for affecting and managing the delivery of health care as well as the concern of the community as a whole. One of the objectives of this paper is to investigate migraine from these two perspectives.
Finally, it is an appropriate time for an OHE publication to examine migraine because of contemporary and indeed, mutually relevant developments in therapeutic research and the NHS. After a prolonged period in which drug therapy for migraine has made little advance, research has produced promising medicines for the effective treatment of acute episodes of migraine. At the same time, the NHS is becoming increasingly concerned to ensure maximum efficiency in the use of its resources. New medicines, along with other forms of intervention, will therefore more frequently be examined from a value for money viewpoint in addition to being subject to conventional clinical assessments. Against the background of these two developments, this paper examines some of the critical issues involved in assessing the economic and quality of life impacts of therapies for migraine.
Blau, J.N. and Drummond, M.F.
(1991) Migraine. OHE Series on Health. Available from https://www.ohe.org/publications/migraine-1/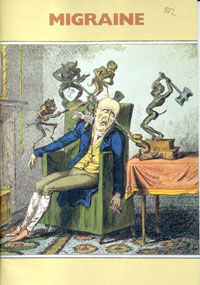
Notifications