Sign up to our newsletter Subscribe
Analysing Global Immunisation Expenditure

Sign up to our newsletter Subscribe


The Office of Health Economics (OHE) and the Swedish Institute for Health Economics (IHE) publish a report evaluating the efficiency of resource allocation in cancer care across Europe. Treatments for and diagnosis of cancer have experienced significant advancement over the…
The Office of Health Economics (OHE) and the Swedish Institute for Health Economics (IHE) publish a report evaluating the efficiency of resource allocation in cancer care across Europe.
Treatments for and diagnosis of cancer have experienced significant advancement over the past few decades. Yet the burden of cancer across an ageing European population continues to grow, whilst in parallel, healthcare systems are facing growing financial pressures.
OHE, in partnership with the Institute for Health Economics (IHE) in Sweden, have just published a report – initiated and funded by BMS – which evaluated the current burden of cancer and identified opportunities for increased efficiency in cancer care. The evidence focused specifically on the health and cancer care landscape in nine European countries (Belgium, Denmark, France, Germany, Italy, the Netherlands, Poland, Sweden, and the UK) as well as the EU27 average.
The report highlights that cancer represents a significant disease burden in Europe: 17% of the total disability-adjusted life years (DALYs) lost are due to cancer. Utilising secondary data, we evaluated country level cancer care spending, and how this relates to disease burden, measured in DALYs.
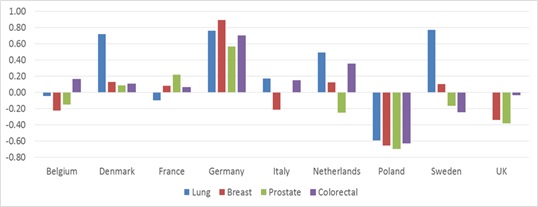
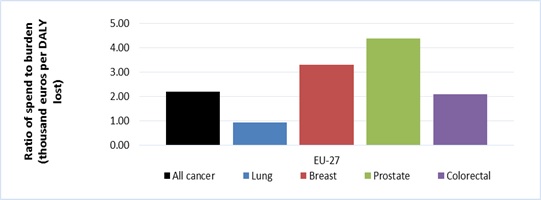
Health care resources allocated to cancer vary substantially by country; Figure A shows that Germany spends significantly more on cancer relative to its burden compared with the European average, whereas Poland spends significantly less than the European average. Across tumour types, spending on lung cancer is significantly lower relative to burden than three other major cancers; with a ratio of spending to burden less than half that of ‘all cancer’ (see Figure B).
Figure A: Spend relative to disease burden compared with the European average for each tumour type (A negative number indicates a lower spend to burden ratio than the European average)
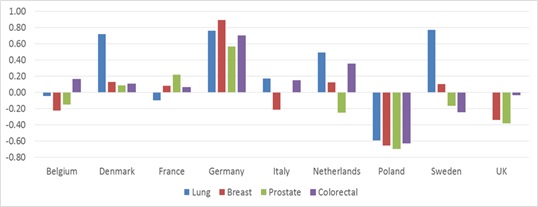
Figure B: Spend relative to disease burden (thousands Euros per DALY lost) by cancer type; EU27 average
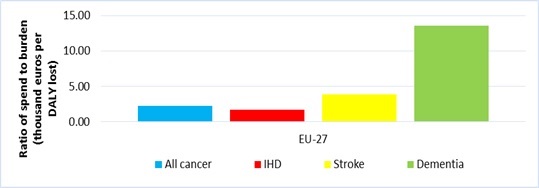
The report acknowledges the importance of resource allocation decisions in the context of the availability of effective and cost-effective treatments in a disease area. However, it is nevertheless pertinent to note the proportionality between spending and burden. Compared with stroke and dementia, spend on cancer is lower relative to burden, only slightly higher than spend on ischemic heart disease (see Figure C).
Figure C: Spend relative to disease burden (thousand euros per DALY lost) by disease – average in EU27
Our analysis of the total economic burden to society looks beyond direct health care costs of cancer and assesses the magnitude of costs borne by cancer patients and society more generally. The direct costs of cancer to the health care system represent less than half of the total cost of cancer to society; ranging between 27% of total costs in Denmark to 42% in Italy.
Production losses from patients no longer being able to undertake paid work are significant, representing between a third and a half of total economic burden depending on the country. This is followed by informal care (the value of care provided by friends and family) and unpaid work (the value of unpaid work a cancer patient can no longer undertake such volunteering or being care givers themselves).
The report found that significant opportunity for improved efficiency exists in prevention activities and early diagnosis, for example targeting unhealthy behaviours such as high alcohol consumption and smoking, and the implementation of quality screening programmes particularly in breast, lung and colorectal cancer.
It is also possible to achieve greater efficiencies in the way we evaluate new treatments, and enhance their uptake. For example, reduced delays in regulatory approval and national-level access could be facilitated through managed entry agreements and the greater exploitation of real-world evidence.
In addition, case study analyses revealed significant possible savings, such as the €7.1 billion that could be saved during the period 2016-2020, through increased generic and biosimilar competition in the oncology market.
Our report has identified several areas where efficiencies – or the way we allocate resources – can be improved. Some of these have the potential to be cost-saving. Other practices may also improve overall efficiency by improving patient outcomes, even if they require additional expenditure. The major challenge for society is to get the balance right: between outcomes for patients, spending and efficiency.
View the short executive summary here.
Download the full report and data compendium here.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!

