Sign up to our newsletter Subscribe
Analysing Global Immunisation Expenditure

Sign up to our newsletter Subscribe


The NICE methods review consultation included a proposal to consider health inequalities more explicitly in their Health Technology Assessment process. But there is still a long way to go before NICE finds a way to tackle all the complexity of…

The NICE methods review consultation included a proposal to consider health inequalities more explicitly in their Health Technology Assessment process. But there is still a long way to go before NICE finds a way to tackle all the complexity of this concept. In the following sections we provide an overall view of the main challenges.
This blog post is the sixth (and last) in a series on the new National Institute for Health and Care Excellence (NICE) health technology evaluation manual. Each post provides a critical discussion on a particular topic, including the expected implications of the changes (or lack thereof) in the manual; what is still missing; and what further research is needed.
The NICE methods review consultation included a proposal to consider health inequalities (HI) more explicitly in their Health Technology Assessment (HTA) process. This proposal is part of a larger commitment to put an increased focus on tackling HI, as one of the key trends and developments in the NICE 2021 to 2026 strategy. NICE has just published the results of a public dialogue on health inequalities (‘NICE listens’), with the aim of identifying people’s views on health inequalities. The report is a good first step towards the identification of the most relevant dimensions that the concept of HI can encompass. But there is still a long way to go before NICE finds a way to tackle all the complexity of this concept. In the following sections we provide an overall view of the main challenges.
What do the public understand by ‘Health Inequalities’?
On the basis of a thorough consultation with the public, the concept of ‘health inequalities’ was articulated as unfair, avoidable, and systematic differences in health outcomes between groups which are determined by circumstances that are largely beyond an individual’s control. This definition is largely shared with other institutions and organisations such as the Institute for Fiscal Studies or Public Health Scotland, although whereas the economic literature uses ‘inequalities’ to denote differences between groups, and ‘inequities’ to denote unfair differences between groups, the definition searched by NICE will adopt the term ‘inequality’ to describe unfair differences.
When are differences seen as ‘unfair’?
This is the trickiest question of all. ‘Unfair differences’ are typically seen by the public as ‘undeserved differences’, indirectly pointing towards a role for individuals’ behaviour (or personal choices) in determining the fairness of health differences. And here comes the key discussion point: to what extent are personal choices influenced by structural characteristics such as social background or where you live? Figure 1 provides a view of the complex mix of societal, environmental, and individual factors that can lead to inequalities in health. A recent survey collected by the Institute for Fiscal Studies and the Nuffield Foundation (‘Attitudes to Inequalities’) found that around one third of the 2,226 British respondents to the survey considers the individual to be fully responsible for their health outcomes (‘individualists’). In other words, individual choices rather than societal and environmental factors are to blame for differences in health and therefore are not unfair. The opposite view is taken by another third of the respondents (‘structuralists’), who put significant weight on economic differences and on inequality of opportunities (including in education and employment) as factors that explain differences in health. As you may have already guessed, the remaining third of the population is in-between ‘structuralists’ and ‘individualists’. You may not have guessed, though, that this segmentation of views cuts across age, gender, social grade, geography, political party affiliations, and Leave/Remain support. Thus, we have one nation with polarised attitudes towards health inequalities. [Note: the results form NICE listens suggest that only a minority of participants (from a total of 28 persons) would fit into the ‘individualists’ group.]
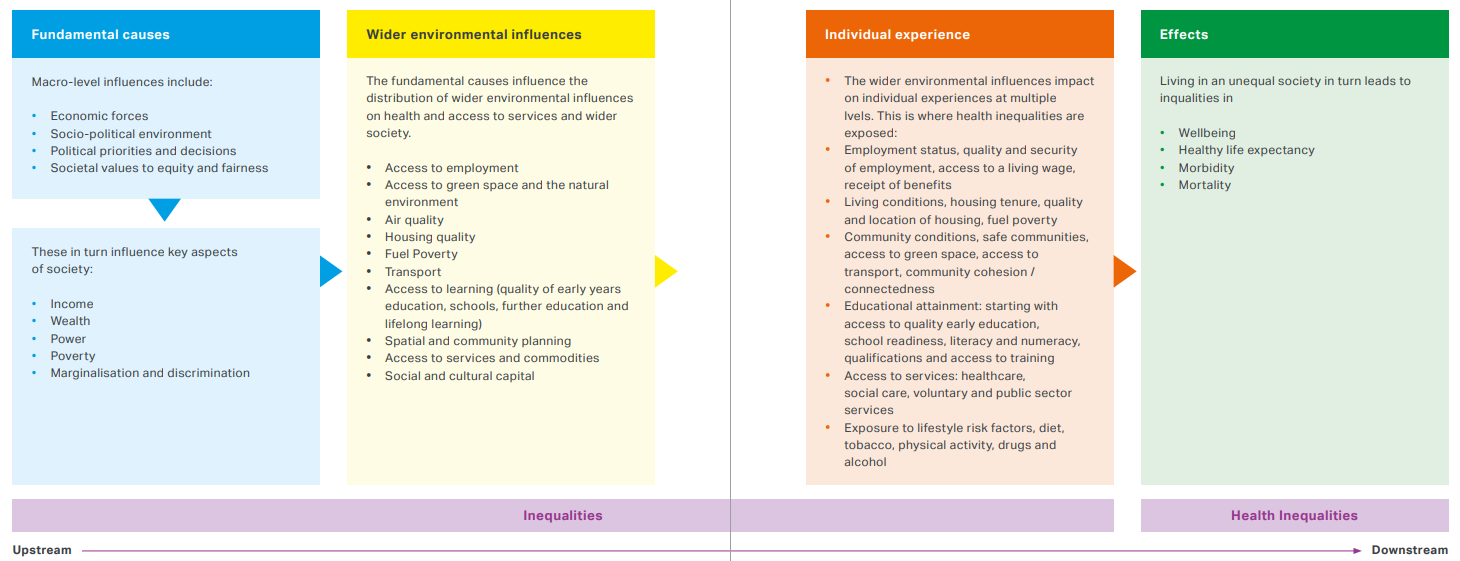 Figure 1: The cause of health inequalities. Source: Cavill, Parker and Hammond (2020) adapted from Public Health Scotland (2021)
Figure 1: The cause of health inequalities. Source: Cavill, Parker and Hammond (2020) adapted from Public Health Scotland (2021)
How should ‘Health Inequalities’ be tackled?
Fortunately, both reports (‘NICE Listens’ and ‘Attitudes to Inequalities’) showed that there is general agreement on two things. First, if unfair group differences in health exist, then there is a need to address them to promote a ‘fair’ society. And second, a holistic approach (going beyond the healthcare system) is essential. The need for governance arrangements involving health and non-health sectors has already been emphasised by the Marmot Review ‘Fair Societies, Healthy Lives’. A cross-sector approach to reduce health inequalities is essential, due to the multiple links between health and individual experience, especially educational attainment, living conditions, and access to services. For example, education is frequently seen as one of the main determinants of health but falls outside the remit of NICE or the NHS. Accordingly, health inequalities can be indirectly addressed from the Department for Education in a number of ways (such as breakfast clubs in schools to increase the learning outcome of students for poorer backgrounds; or Education and Health Care Plans (EHCP) for children with special educational needs). Tackling inequalities requires direct collaboration across public sector departments and even across councils, but suboptimal cooperation means populations in need fall through the cracks of the system, leading to greater inequalities. A timely example for this is well described in this article at The Economist, addressing HI related to health and education support for children with Autism Spectrum Disorder, and concluding that “only parents who are educated, know their children’s rights and can afford lawyers (…) are able to navigate the system”.
Then, what part of ‘Health Inequalities’ is in the remit of NICE?
NICE is responsible for improving outcomes for people using the NHS, public health services and social care services. Therefore, NICE can tackle inequalities in health outcomes associated to environmental or individual factors within the remit of health care, public health, and social care services. From Figure 1, we could think of interventions related to access to services, and education around (and exposure to) lifestyle risk factors. For instance, health inequalities arising by the ‘postcode lottery’ in the access of in vitro fertility services fits very well there.
And what is on the remit of HTA?
As noted, HI are a multi-factorial problem, overlapping with education, employment, income, housing, and so on. Therefore, the opportunity of HTA to address this seems quite limited. Reducing inequalities in the access to treatments is probably the most prominent line of action in the remit of HTA (see individual experience in Figure 1). For instance, introducing a HI modifier may be an extension of the policy for rare diseases – as the severity modifier was meant to be an extension of the policy tackling with inequalities in access to treatment at the end of life.
Overall, we may all agree that clinically and cost-effective technologies that exacerbate health inequalities should not be recommended. Now, let’s see how we can agree on how to systematically operationalise this. OHE is looking forward to seeing NICE’s proposals on this line of research. Let’s do it!
Related research
Cubi-Molla, P., Buxton, M. and Devlin, N., 2021. Allocating public spending efficiently: is there a need for a better mechanism to inform decisions in the UK and elsewhere? Applied Health Economics and Health Policy, 19(5), pp.635-644. DOI: 10.1007/s40258-021-00648-2
Asada, Y., Abel, H., Skedgel, C. and Warner, G., 2017. On effective graphic communication of health inequality: considerations for health policy researchers. The Milbank Quarterly, 95(4), pp.801-835. DOI: 10.1111/1468-0009.12300
Related blogs
A series on the new National Institute for Health and Care Excellence (NICE) health technology evaluation manual
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!



