Sign up to our newsletter Subscribe
Analysing Global Immunisation Expenditure

Sign up to our newsletter Subscribe


In this article, we discuss the global issue of drug shortages. We summarise our research where we developed a framework for quantifying the cost of a shortage, and through three case studies provide illustrative estimates of these costs.

What are the impacts of a drug shortage? Who is affected? And how significantly?
Our latest research report answers these questions and helps policy-makers understand a key trade-off facing health systems around the world: increasing pressure to lower prices of generic and biosimilar medicines, versus the rising tide of drug shortages.
As our previous research (Napier et al., 2024) identified, drug shortages occur most significantly in markets of off-patent generic medicines and biosimilars. This is mainly the result of cost containment policies resulting in heavy price erosion and commercially unattractive markets for these drugs. Few producers are incentivised to supply those markets which therefore lack resilience and bandwidth to deal with demand shocks or supply issues, making them more vulnerable to shortages.
To better understand this trade-off, we provide a framework to estimate the cost of a drug shortage. Through a series of hypothetical case studies, we apply this framework to demonstrate the potential scale of those costs, and who bears them.
Patient health impact. Healthcare systems resource use. Drug acquisition cost.
These are the elements of the cost of drug shortage framework we developed, shown below in Figure 1. The patient impact may include delays in receiving treatments, receiving less effective alternative care, drug prescribing errors and poorer patient adherence (De Weerdt et al., 2017; Nonzee and Luu, 2019; Phuong et al., 2019).
In addition, drug shortages can impact the prices of the drugs themselves in shortage, as well as their substitutes. A study in the US estimated price increases resulting from shortages to be responsible for $230 million in additional costs in 2018 (Hernandez et al., 2018).
Impact on healthcare resource use includes the cost of managing drug shortage disruptions, and the opportunity cost of this time. The impact of this consequence on the US health system, for example, is estimated to be $359 million (2019 estimate) (ASPE, 2023).
However, with the incidence of drug shortages being much higher in recent years (Napier et al., 2024), we expect both the impact of price increases and additional healthcare resource use at the aggregate level to be significantly greater than these estimates.
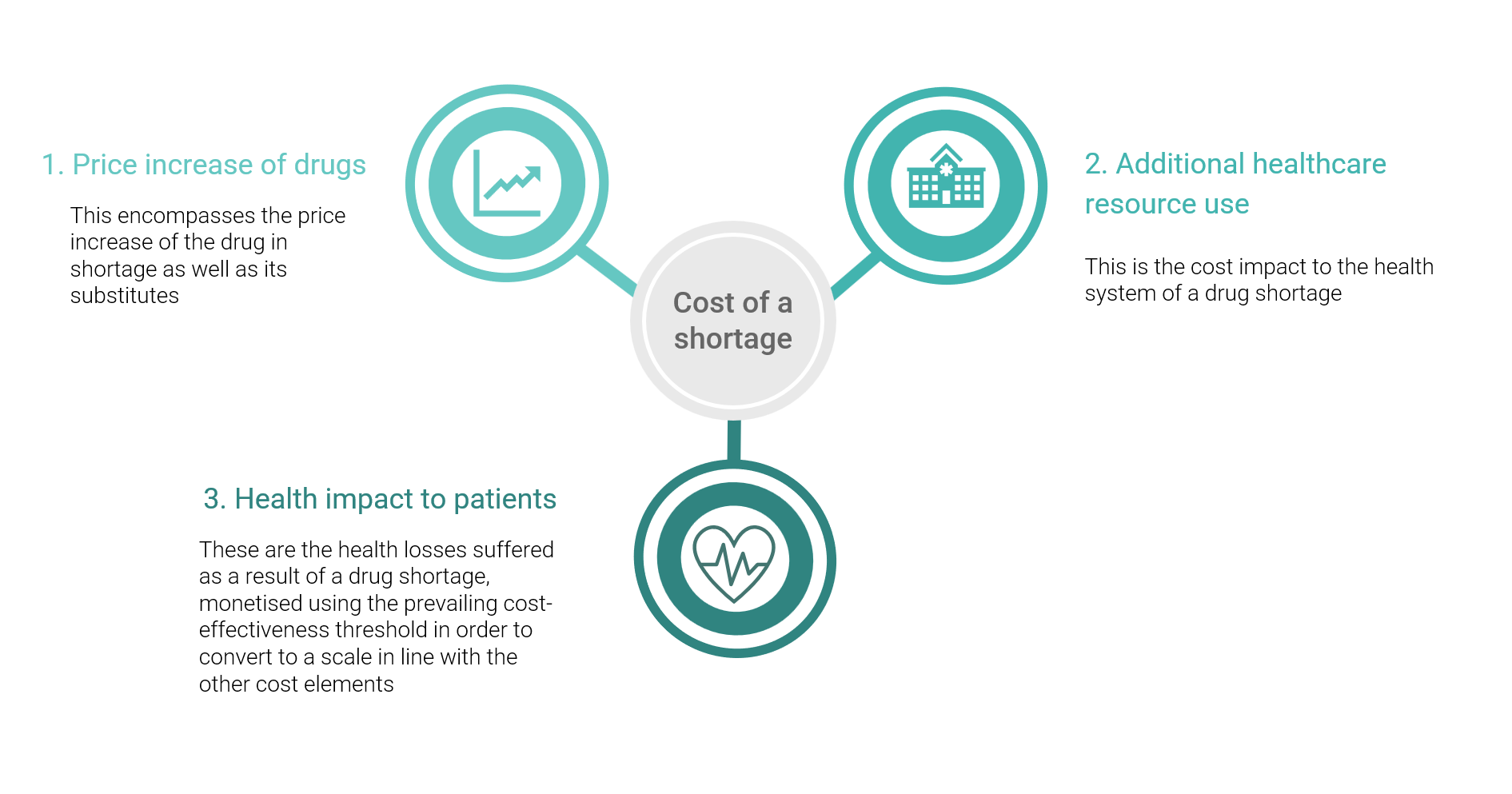
Figure 1 – Cost of Drug Shortages Framework
To explore how the impacts of drug shortages may differ, we applied the framework to three separate illustrative (hypothetical) case studies: Trastuzumab, Statins, and Saline. They were selected to show the varying impact different types of drugs (a biosimilar, a small molecule generic, and a generic injectable), used to treat very different patient groups, may have.
A shortage of Trastuzumab could result in significant patient health losses.
Trastuzumab is a highly effective biologic used in the treatment of early-stage HER2-positive breast cancer, as well as other cancers (Cancer Research UK, 2024). Although no significant shortages of trastuzumab have yet been reported, shortages of other biosimilars have been reported in Europe.
In the early-stage HER2-positive breast cancer population, we estimated that in the US a Trastuzumab shortage could amount to $450 million in health losses. This is driven by the lack of access to treatment when a shortage occurs, and patients receiving the less effective previous Standard of Care (SOC). We converted the resulting loss in Quality Adjusted Life Years (QALYs) into monetary terms using the most appropriate prevailing estimate of the cost-effectiveness threshold in this setting.
We found a lower (but still significant) cost from an EU perspective of €16.2 million. This difference was driven by a currently shorter average duration of drug shortages, more patients being able to switch to alternative trastuzumab products, and a lower threshold applied for the “value of a QALY” in the EU.
A shortage of Statins would have high monetary impacts
Statins are small molecule therapies used to lower cholesterol and reduce the risk of heart and blood vessel disease, with large populations taking Statins in both the EU and US. No significant shortages of any individual statin have yet been reported. Unlike Trastuzumab, we would expect negligible health losses as a result of a shortage, as there are many producers of different statins with therapeutic equivalence (Zhou et al., 2022; Jacobson et al., 2013).
We considered the impact of a hypothetical shortage of a particular statin, finding in the US setting that high costs would be driven by price increases of the drug in shortage and its competitors: $1.4 billion (high due to the huge population this shortage would affect). From the EU perspective, evidence of price changes resulting from drugs in shortage is scarce. Rather, modelled costs were driven by the health system disruption that would result from a shortage, amounting to €63 million.
Saline shortages cause huge disruption to the health system.
Saline has a wide variety of uses and is a key part of the medical supply for hospital-based care, including fluid resuscitation, intravenous therapy, and wound irrigation (DoveMed, 2023). Unlike Statins and Trastuzumab, there have been widespread reports of Saline shortages, in a market characterised by very low prices and few competitors.
Saline’s extensive use in hospitals means that vast numbers of healthcare staff and patients are affected. Many academic and news articles describe the hugely resource-intensive processes involved in managing Saline shortages (Mazer-Amirshahi and Fox, 2018; Crow, 2018).
The impact of ‘muddling -through’ saline shortages to minimise their impact on care takes a huge toll on staff and ultimately the ability of the health system to run effectively and efficiently. Although we could not precisely estimate the cost of a Saline shortage, due to its broad use across many elements of hospital care, we expect the overall cost to be extremely high. Furthermore, the frequency of those shortages are compounding the cost borne by health systems.
Policymakers need to weigh the control of expenditure against the cost of shortages.
The costs to society of drug shortages are likely to be very large. Our research contributes a framework to estimate the make-up and magnitude of those costs. Through three case studies we have demonstrated that those costs will be very disparate in nature and size depending on the drug impacted.
Despite the significant cost estimates, it is likely that we are omitting some important factors in our case studies, such as legal costs in the US, as well as the extent of adherence impact when switching to alternative treatments, particularly in the statin case study.
Since drug shortages are becoming more commonplace, we are likely as a society to observe the rising consequent harm to patient health, healthcare systems and healthcare budgets.
While policy-makers exert efforts to control pharmaceutical expenditure with cost-containment policies, greater consideration must be given to the downstream impact this may cause to vulnerable supply chains and higher risks of shortages, particularly in the generics and biosimilars market which already only represents around 3% of total healthcare expenditure (AAM, 2022). By demonstrating the nature and scale of the impact of drug shortages, we urge policy-makers to consider this trade-off, to promote sustainable drug markets and resilient supply chains for the benefit of all stakeholders and society as a whole.
For more detailed analyses of the topic, please read our report here.
AAM, 2022. Report: 2022 U.S. Generic and Biosimilar Medicines Savings Report | Association for Accessible Medicines. [online] Available at: https://accessiblemeds.org/resources/reports/2022-savings-report [Accessed 10 Sep. 2024].
ASPE, 2023. ASPE Report to Congress: Impact of Drug Shortages on Consumer Costs. [online] ASPE. Available at: https://aspe.hhs.gov/reports/drug-shortages-impacts-consumer-costs [Accessed 13 Dec. 2023].
Cancer Research UK, 2024. Trastuzumab. [online] Available at: https://www.cancerresearchuk.org/about-cancer/treatment/drugs/trastuzumab [Accessed 13 May 2024].
Crow, D., 2018. Saline investigation highlights the cost of American healthcare. [online] Available at: https://www.ft.com/content/4593b93e-1887-11e8-9376-4a6390addb44 [Accessed 18 Mar. 2024].
De Weerdt, E., Simoens, S., Casteels, M. and Huys, I., 2017. Clinical, Economic and Policy Implications of Drug Shortages in the European Union. Applied Health Economics and Health Policy, 15(4), pp.441–445. 10.1007/s40258-016-0264-z.
DoveMed, 2023. Normal Saline: Uses, Composition, Administration, and Considerations. [online] DoveMed. Available at: https://www.dovemed.com/health-topics/focused-health-topics/normal-saline-uses-composition-administration-and-considerations [Accessed 10 Apr. 2024].
Hernandez, I., Sampathkumar, S., Good, C.B., Kesselheim, A.S. and Shrank, W.H., 2018. Changes in Drug Pricing After Drug Shortages in the United States | Annals of Internal Medicine. [online] Available at: https://www.acpjournals.org/doi/abs/10.7326/M18-1137 [Accessed 3 Jan. 2024].
Jacobson, T.A., Wertz, D.A., Kuznik, A. and Cziraky, M., 2013. Cardiovascular event rates in atorvastatin patients versus patients switching from atorvastatin to simvastatin. Current Medical Research and Opinion, 29(7), pp.773–781. 10.1185/03007995.2013.802229.
Mazer-Amirshahi, M. and Fox, E.R., 2018. Saline Shortages – Many Causes, No Simple Solution. The New England Journal of Medicine, 378(16), pp.1472–1474. 10.1056/NEJMp1800347.
Napier, M., Kourouklis, D., Cole, A. and Cookson, G., 2024. The Dynamics of Drug Shortages. [online] OHE – Leading intellectual authority on global health economics. Available at: https://www.ohe.org/publications/the-dynamic-of-drug-shortages [Accessed 10 May 2024].
Nonzee, N.J. and Luu, T.H., 2019. The Drug Shortage Crisis in the United States: Impact on Cancer Pharmaceutical Safety. In: J.M. McKoy and D.P. West, eds., Cancer Policy: Pharmaceutical Safety, Cancer Treatment and Research. [online] Cham: Springer International Publishing, pp.75–92. 10.1007/978-3-319-43896-2_6.
Phuong, J.M., Penm, J., Chaar, B., Oldfield, L.D. and Moles, R., 2019. The impacts of medication shortages on patient outcomes: A scoping review. PLOS ONE, 14(5), p.e0215837. 10.1371/journal.pone.0215837.
Zhou, Z., Curtis, A.J., Ernst, M.E., Ryan, J., Zoungas, S., Wolfe, R., McNeil, J.J., Murray, A.M., Reid, C.M., Chowdhury, E.K., Woods, R.L., Tonkin, A.M. and Nelson, M.R., 2022. Comparison of statins for primary prevention of cardiovascular disease and persistent physical disability in older adults. European Journal of Clinical Pharmacology, [online] 78(3). 10.1007/s00228-021-03239-1.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!



