Sign up to our newsletter Subscribe
Analysing Global Immunisation Expenditure

Sign up to our newsletter Subscribe


We dust off last year’s model to consider the potential savings to the NHS from more people going vegan, with a focus on COVID-19.

As we near the end of another Veganuary, we’re revisiting and updating previous OHE research exploring the potential impact of a higher uptake of plant-based diets in England. Last year, we published a model-based analysis which found that if the entire population of England adopted a plant-based diet, the estimated healthcare cost savings to the NHS from a lower incidence of chronic diseases could total around £6.7 billion per year. The population could benefit from over 2 million fewer cases of disease, corresponding to an additional 172,735 quality-adjusted life years (QALYs).
We conducted a literature review to identify health conditions for which a statistically significant difference in the relative risk (positive or negative) of experiencing the health condition existed for vegan compared with non-vegan diets. For each condition identified, we extracted quantitative estimates relating to the i) prevalence, ii) health care costs, and iii) health state utility value (HSUV) associated with the condition. We identified relevant evidence relating to cancer, coronary heart disease, cataracts, diverticular disease, bone fractures, stroke, and type 2 diabetes and selected the most relevant estimates for the population of England.
What’s new?
Since then, new research has been published that highlights the association between adoption of plant-based diets and COVID-related outcomes. In fact, it was only the day after last year’s Insight that Acosta-Navarro and colleagues published a study showing lower incidence of COVID-19 infection for people consuming plant-based diets in Brazil (Acosta-Navarro et al. 2024). For several years, early evidence has demonstrated possible benefits of a plant-based diet for COVID risk, with researchers suggesting that the mechanism could relate to more consumption of immunity-boosting nutrients and relevant protease inhibitors (Soltanieh et al. 2023). More significant for our study was the publication of a systematic review and meta-analysis by Papadaki and colleagues, first published in May 2024.
Papadaki and colleagues report the risk of both COVID-19 infection and COVID-19 hospitalisation, deriving evidence from a total of 649,315 participants across seven studies. Headline findings include plant-based diets being associated with a 59% reduced risk of infection in case-control studies and an 18% reduction in risk in cohort studies, with a 62% lower risk of hospitalisation. There is no doubt that more research is needed, but these are strong signals.
It’d be great to include this in our model, but there’s a problem. Our model is designed to consider chronic health conditions. So what about long-COVID? We don’t have direct evidence yet, but it’s reasonable to infer that lower COVID infection rates are associated with a lower risk of long-COVID. What’s more, severe cases of COVID are more likely to lead to long-COVID, and plant-based diets appear to be associated with reduced severity.
Incorporating COVID
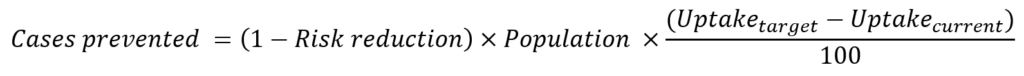
To calculate the total cases prevented per disease, we use the current prevalence of the disease, the relative risk of experiencing that disease to an individual with a plant-based diet, the difference between target plant-based population and the current plant-based population.
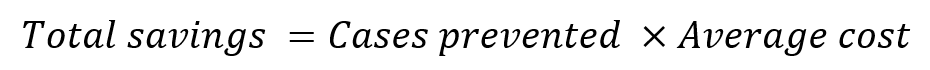
To calculate the healthcare cost savings per disease, we use the total cases prevented and the average cost to the NHS of treating a person with that disease.
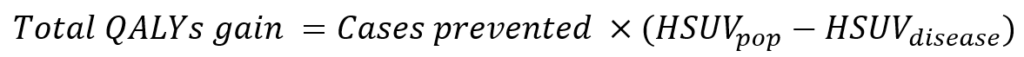
To calculate the total QALYs gained per disease, we use the total cases prevented, the HSUV
population norm and the HSUV of the disease.
As described above, we need to infer long-COVID rates from the risk of COVID infection. Using the most conservative estimates we can find, let’s assume the following parameters for the inclusion of long-COVID:
Adding these parameters to our model estimates an additional annual saving to the NHS of £184 million, with 177,681 fewer cases of long-COVID and a gain of 9,950 QALYs. If we consider the 59% risk reduction from Papadaki et al, the savings balloon to more than £600 million, with 582,400 fewer cases.
Beyond chronic disease
Our model presents a simplified view of the world, capturing only the long-term effects of chronic diseases. Even in incorporating COVID into our model, we exclude the short-term costs of hospitalisation following infection, which are likely to be the dominant drivers of costs associated with COVID.
The pandemic has helped to reveal the importance of diet for people’s infection risk, and a more dynamic modelling exercise would be needed to fully capture benefits. Here at the OHE, we’ve spent a lot of time researching the value of prevention with interventions such as vaccines, which can have broad impacts on population health and the wider economy (El-Banhawi et al. 2024; Brassel et al. 2020). Dietary changes may bring similarly huge benefits, but we lack the necessary data to fully explore these questions.
Plant-based diets also have important implications for infectious disease beyond the prevention of individual infections. The COVID-19 pandemic brought the notion of zoonotic disease into public discourse, and meat production is contributing to the risk (Koren et al. 2024). Antimicrobial resistance (AMR) is currently regarded by the World Health Organization (WHO) as one of the most significant risks to global public health. The use of antimicrobials in animals has contributed significantly to the development of AMR in humans (Allel et al. 2023). Reducing meat consumption should be seen as part of the solution (Van Boekel et al. 2017).
And the benefits extend beyond health. Our model does not account for the environmental impact that would result from wider adoption of plant-based diets. A recent study of vegans, vegetarians, fish-eaters and meat-eaters in the UK found that the dietary impacts of vegans are around a quarter of high meat-eaters for greenhouse gas emissions and land use, less than half for water use, and around a third for biodiversity (Scarborough et al. 2023).
What now?
While 100% uptake of vegan diets in the UK may seem ambitious, such a dramatic shift in the population’s health behaviours could result in transformative changes for individuals, the NHS, and the planet. It won’t be possible for us to accurately measure and fully account for all benefits.
In some countries, the evidence is proving strong enough, and we are seeing strong commitments to plant-based food policies. Denmark’s Action Plan for Plant-Based Foods is one of the most visionary strategies to date. We recently attended an event in parliament hosted by the Vegetarian Society, where Rasmus Prehn (Danish MP and former Minister for Food, Agriculture and Fisheries) and Rune-Christoffer Dragstahl (Secretary-General of the Danish Vegetarian Society) explained how government led collaboration involving key stakeholders can drive positive change and support relevant industries on this path to a healthier and more sustainable future.
Our analysis last year was supported by the Vegan Society;
This is even more evidence of the fact that veganism can pay huge health dividends. Policymakers must follow the visionary examples of countries such as Denmark, which have begun to embrace and encourage plant-based foods and diets, and include support for these in the Government’s upcoming Food Strategy and NHS 10 Year Plan – not only to free up billions of pounds of funding to invest back into England’s hospitals and services – but also to tackle the joint health and sustainability crises and enable people to live longer, healthier lives.
The pre-print version of the report is published on medRxiv: “The impact of higher uptake of plant-based diets in England” and you can explore the results and generate estimates using your own inputs with our interactive web app.
For more information and resources about switching to a vegan diet, visit vegansociety.com.
This research was independently funded by the OHE. It builds on our model-based analysis from 2023 study, commissioned by the Vegan Society, which showed that with 100% adoption of plant-based diets in England, total health care cost savings for the NHS could be around £6.7 billion.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!