Sign up to our newsletter Subscribe
Challenges and Solutions for Budget Impact Analysis of Gene Therapies

Sign up to our newsletter Subscribe

OHE held a webinar expanding on the findings and recommendations outlined in the recent whitepaper report. The event brought together experts from government, industry, and academia to share insights, focusing on strategies aimed at spearheading a transformative era of prevention.

Reimagining prevention
With only 5% of NHS funding being allocated to preventative care between 2013 and 2019 (ONS, 2022), it is clear that despite substantial evidence of the value of prevention, significant barriers remain.
The OHE report, ‘Reimaging Prevention for a Healthier, More Prosperous Society’ outlines the economic and health benefits resulting from prevention and offers key recommendations for stakeholders to collaborate in ushering in a new era of commitment to prevention. Panellists were asked to comment on the recommendations in the report and provide an overview of prevention related work ongoing in their respective organisations.
How are key stakeholders supporting the prevention agenda?
Industry
Our first panellist was Dilruwan Herath, an accomplished medical affairs leader with 16 years of experience in the pharmaceutical industry. He opened with a summary of the UK’s history of success in public health initiatives, exampling how uptake of HPV vaccinations has rendered the likelihood of cervical cancer as almost negligible. However, he noted that such advancements in prevention are often dismantled due to political change, leading to reductions in investment and resources. This is worsened by the lack of adaptability found in the delivery of public healthcare, as revealed, and aggravated by the pandemic.
Despite the resource limitations faced by the NHS, he restated the necessity of prioritising funding for preventative avenues that can optimise efficiency. Considering the role of the pharmaceutical industry, Dilruwan suggested that industry could explore variations of funding streams as a practical way to support and reimburse preventative initiatives. Additionally, strategic plans across different areas need to be aligned to cultivate a centralised and constructive plan that goes beyond vaguely alluding to commitment in public policy statements. Ultimately, the pharmaceutical industry needs to work alongside preventative projects and actively contribute to advancements.
He also raised a point surrounding the benefits of postgraduate learning investment. He argued that this could successfully mitigate the influence of political opinion on prevention activities by equipping future Healthcare Professionals to make informed decisions about the services they deliver.
Finally, Dilruwan pointed to the value of maximising advances in technology to enhance real time data for better monitoring, optimising precision public health. He also suggested implementing interventions prior to waiting for full data sets, by casting predictions with limited but strong and robust data sets.
Northern Health Science Alliance (NHSA)
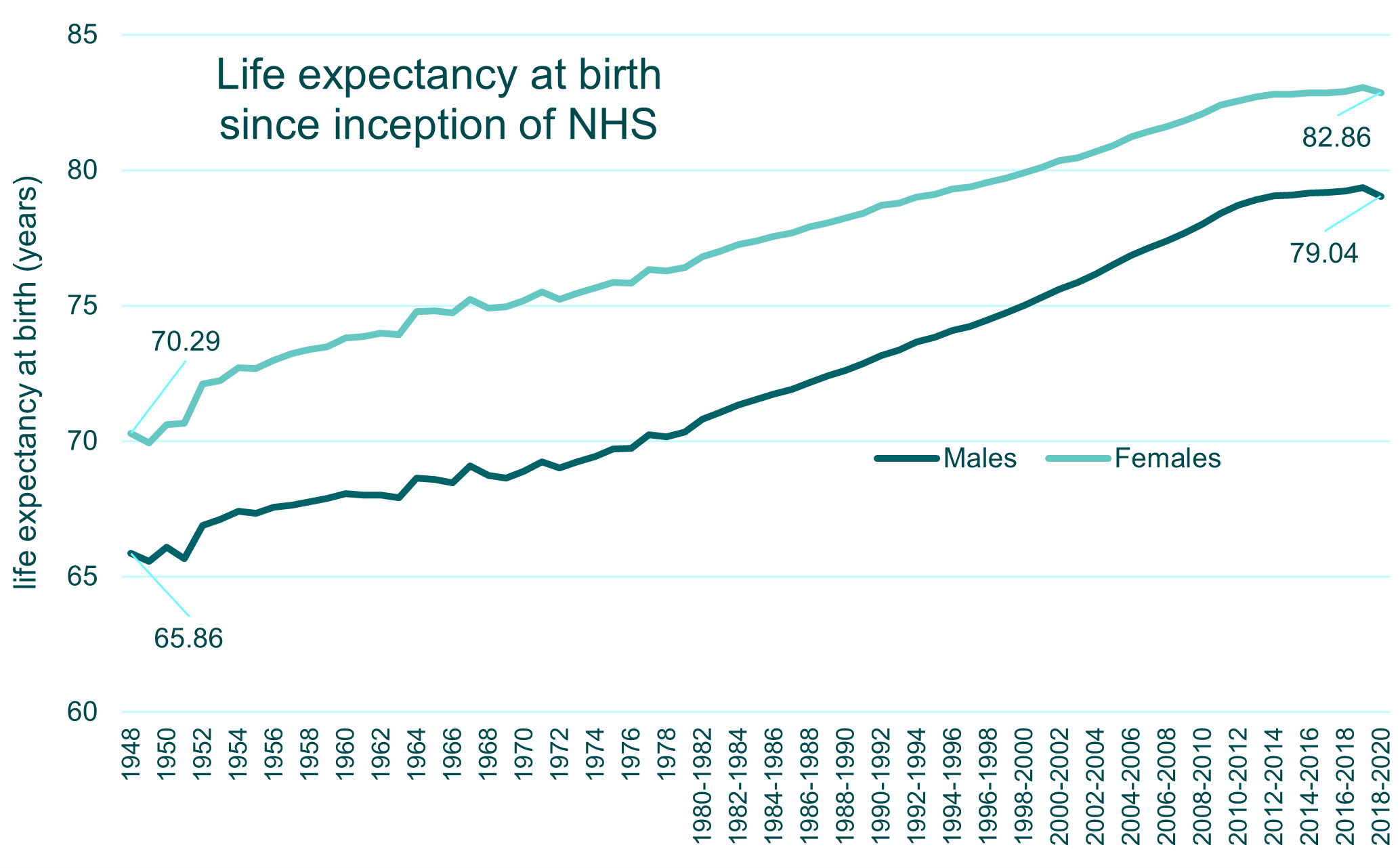
Our second speaker was Hannah Davies, Executive Director and Health Inequalities Lead at the NHSA, which unites health and life science expertise within the NHS and academia. To set the scene for the extent of the discrepancy in health equity between the north and the south, she shared that the average life expectancy in the North is 2 years lower than in the South.
The NHSA’s ‘Child of the North’ report is imperative to building an understanding of where and how inequity begins, to better inform targeted prevention initiatives. Advocating for intervention earlier in the life course facilitates detection and treatment access. Providing adequate early support avenues will reduce the burden on struggling local authorities, ultimately reducing adversity.
Hannah called for careful consideration of accessibility to ensure that the intended communities are engaged with interventions to make a tangible difference to the trajectory of their health. Given that the predominant precursor of poor health is exposure to health damaging environments stemming from poverty, policy actions should strive to advance these determinants of health. This could include increasing funding to community focussed prevention services within children’s centres, family hubs and early help centres.
Echoing some of the recommendations from the report, she noted the necessity of an efficient national strategy that focalises on communities most at risk, allocating investment funds proportional to need. This is why entities such as the NHSA are crucial to monitor the extent of geographic discrepancies, revealing the populations at highest risk of health inequity.
Government
Our final panellist, Clare Perkins, Deputy Director of Personalised Prevention in the Office of Health Improvement and Disparities, UK Government, provided a national perspective on the prevention agenda.
She gave examples of national action prevention initiatives, such as the ‘Healthier You’ programme, which offers people a choice between accessing digital or in person programmes that facilitate and encourage lifestyle changes.
Clare added that the government is investing up to £645 million in expanding prevention services over the next two years, which includes £17 million in digitising the NHS health check, which is part of a wider strategy to shift the delivery of prevention services closer to where people live, work, and socialise. Use of data and behavioural insights enable us to target and tailor health campaigns to specific communities through identifying and operating within digital channels that they tend to use. Enhancing health information also fosters a culture of being in control of one’s health and capacity to support self-care management. The benefits of large scale prevention extend beyond health, ultimately benefitting the economy, the individual and contributing to cultural shifts in embedding preventive approaches into population values and behaviours. Whilst a move to digitisation provides the opportunity to deliver personalised prevention at scale, we need to be mindful of the 10 million people estimated to lack adequate digital literacy skills, and ensure that digital advancements are accompanied by literacy programmes to mitigate risks of worsened health inequality.
The forthcoming Major Conditions Strategy (Spring 2024) will outline plans for prevention. This strategy has been co-developed with clinicians, the voluntary sector, and people with lived experience. Clare noted the importance of this shared endeavour for prevention that must extend beyond the realms of the NHS, into all facets of the community.
Audience insights and reflections
The webinar provoked audience questions surrounding the added value of more national policies and interventions, as well as the role that industry should play.
Hannah argued that the Government needs to adopt a ‘health first’ approach to inequalities, as improving equity contributes to both the prevention agenda and the critical success of the country. Pragmatic steps include designing and funding interventions in the areas with most need.
Dilruwan shared the frustration within industry at the lack of long-term strategy, noting that policy change is volatile and unfortunately results in fragmented projects. Thus, he argued that aligning a cohesive voice, sharing insights, and thinking about the bigger picture via a coherent and delivery focused strategy could help formulate successful initiatives.
Another question enquired about successful international efforts to reduce health inequality. The panel agreed that the Scandinavian healthcare system’s achievements in optimising early child and population health are a good example. Hannah listed better equity in childcare and workplace engagement as multiplying effects that might underpin this.
However, Dilruwan warned that although there are great international examples, we cannot ensure that population needs are the same everywhere. Instead, keeping momentum for overarching strategies that integrate solutions to multiple conditions could be the optimal way to address and prevent comorbidities. This alludes to the value of adopting a holistic view to health, encompassing the interplay between multiple indicators and conditions rather than preventing or treating one disease in isolation.
Clare noted that although we know what works well for certain types of prevention (e.g., drugs for cardiovascular disease prevention), we do not necessarily have the same understanding of who individual interventions work for. She called for evidence to address this gap in understanding to enhance our knowledge of what works optimally for which specific group.
You can read some of the questions that were unanswered during the live session below:
Q1: How should preventative care organisation be structured? Top-down or bottom up?
Clare: Both, it requires good leadership at the top and ambition with overarching targets set out in operational guidance, then how this is achieved should be determined locally with enough flexibility for local priority setting
Q2: The evidence, plans and ambitions for prevention are in place. Why do you think only 5% of the NHS budget is allocated to funding prevention? How can we increase allocation?
Clare: I don’t think that it is just the NHS and local government who should be funding prevention, the benefits of prevention are enjoyed across society and therefore keeping people well needs to be a shared endeavour across individuals, the public, private and voluntary sectors. Any increase in prevention spend in the NHS will need to happen gradually over time and be realised from doing things differently.
Q3: there any examples of ‘low hanging fruits’ in terms of well-understood prevention policies or interventions, which are currently not sufficiently leveraged in the UK but could lead to relatively quick benefits to population health. And what are the barriers to effective implementation of these low hanging fruits in the UK?
Clare: On secondary prevention, there are at least 4m people with undiagnosed hypertension, the biggest risk factor for stroke and about a third of people with diagnosed hypertension are not optimally managed. There are cost-effective drug therapies for hypertension, we need to find and manage people better which includes looking at different ways to deliver diagnosis and treatment services e.g. blood pressing testing in community pharmacy.
OHE would like to thank the panel for contributing their insights on this important topic. We invite our audience to join us in our ongoing endeavour to mobilise the prevention agenda as we transition into a more resilient future for healthcare.
Change Initiative
The Change Initiative is uniting organisations across the health and life science sector to address critical global challenges. Preventative Health and Reimagining the Health System is a core research fund topic for the coming years, and we are pleased to have supported this webinar through the Initiative’s activities. If you are interested in learning more about the Change Initiative, please contact cashton@ohe.org.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!