Our literature review suggests that there are more than 100 inequalities impacting on people living with dementia and their carers across multiple characteristics, circumstances, and in various parts of the health and care system. However, the current low availability and quality of data is a major barrier to accurately measuring these inequalities. With the expectation that 1 in 2 people will be affected by dementia during their lifetime, there is a pressing need for further research to inform future policy, research, and service interventions.
Key takeaways
- Our literature review identified 110 inequalities for people affected by dementia in England, Wales, and Northern Ireland.
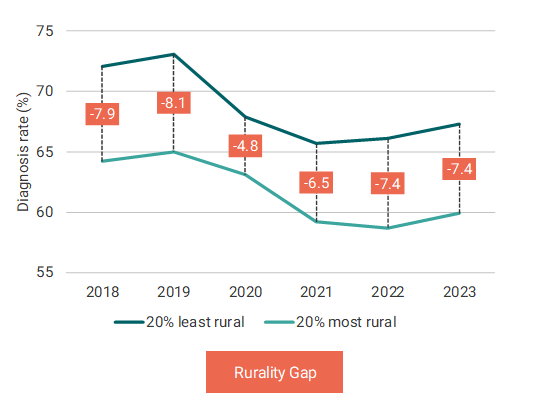
- Inequalities across people living with dementia included those linking location, deprivation, socioeconomic status, age, culture, and ethnicity of people living with dementia with access to and experience of diagnosis and healthcare, A&E attendances and hospital admissions, inclusion in clinical trials, and drug prescribing. For example, diagnosis rates are between 5 and 8 percentage points lower in rural areas, with this gap increasing since 2020.
- Inequalities of informal carers of people living with dementia mainly relate to gender, financial pressures, health and well-being, and health system structural issues. For example, 41% of informal carers of people living with dementia experience financial difficulties, and around 20% are out of the labour force due to caring responsibilities.
- Improving the quality and availability of dementia data collection and publication, and increasing quantitative research is paramount to robustly establish the presence and monitor changes in inequalities in dementia.
An estimated 982,000 people in the UK are living with dementia, expected to rise to 1.4 million by 2040. This high prevalence means that approximately 1 in 2 people will be affected by dementia (that is, living with dementia, or being the informal carer of someone living with dementia) during their lifetime. Improving our understanding of inequalities in the context of dementia is not only desirable, but also necessary to achieve one of the four core purposes of Integrated Care Systems established by NHS England in 2022 (tackling inequalities in outcomes, experience, and access), as well as a central part of the NHS Long Term Plan.
This report deepens understanding of the inequalities that people living with dementia and their informal carers experience from diagnosis to end of life across England, Wales, and Northern Ireland. We identified and assessed the quality of current evidence on inequalities and explored ways to quantify the magnitude and variation of a selection of these inequalities.
Our literature review identified 110 inequalities for people affected by dementia: 82 inequalities related to health care and social care were found for people living with dementia, and 28 inequalities related to health, health care, and social care were found for informal carers of people living with dementia.
We present four case studies related to inequality measurements. Each case study contains a summary of the evidence retrieved from the literature; a recommended potential way to measure the inequality over time using data in England; a discussion of the data limitations and the validity of the proposed measure; and recommendations to improve the measurement with data which are not publicly available or currently collected.
For example, we proposed the ‘rurality gap’ (gap in diagnosis rates between the most and least rural areas) and the ‘concentration index’ (the extent to which diagnosis rates are distributed disproportionately between less or more rural areas). The rurality gap suggests that diagnosis rates are between 5 and 8 percentage points lower in rural areas (see figure below). The rural gap measure fluctuated over time; however, the gap seems to be increasing since 2020. This relationship between lower diagnosis rates and more deprived areas and the evolution over time is consistent with the concentration index results and other studies.
Figure 1 Average diagnosis rates in the 20% most and least rural groups
We also explored financial pressures for informal carers as a result of funding care to meet complex needs and/or leave work to provide informal care, compared to the general population. We found evidence that about 41% of informal carers of people living with dementia experience financial difficulties, and around 20% are out of the labour force due to caring responsibilities (the percentage radically increases from 20% to 53% in 2021-22).
This report highlights important research gaps that need to be filled to improve the understanding of inequalities in dementia, as well as the need to develop robust measures for a set of priority inequalities in dementia. These are essential steps to allow for inequalities in dementia to be effectively tackled.
‘Inequalities in Dementia: Unveiling the Evidence and Forging a Path Towards Greater Understanding’, was commissioned and funded by Alzheimer’s Society.