Sign up to our newsletter Subscribe
Analysing Global Immunisation Expenditure

Sign up to our newsletter Subscribe


OHE’s Sarah Karlsberg Schaffer presented at the Glasgow Health Economics Seminar Series the results of a paper on the value of the cost-effectiveness threshold in Scotland. In November, OHE’s Sarah Karlsberg Schaffer presented at the Glasgow health Economics Seminar Series…
OHE’s Sarah Karlsberg Schaffer presented at the Glasgow Health Economics Seminar Series the results of a paper on the value of the cost-effectiveness threshold in Scotland.
In November, OHE’s Sarah Karlsberg Schaffer presented at the Glasgow health Economics Seminar Series (GhESS) the results of a paper on the value of the cost per quality-adjusted life year (QALY) threshold in Scotland.
The paper, written with Jon Sussex, Nancy Devlin and Andrew Walker, and recently published in Health Policy, tests the feasibility of estimating the “true” cost per QALY threshold using information on the cost-effectiveness of “marginal” services in NHS Scotland – those planned to receive significant investment or disinvestment in the coming financial year. It also explores how the NHS makes spending decisions and the role of cost per QALY evidence in this process.
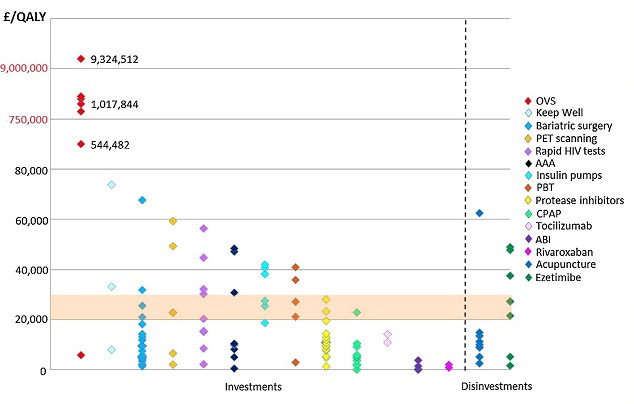
The first key finding presented by Sarah was that the cost-effectiveness of marginal services varies hugely, as is evident from Figure 1 (below). For this reason, the authors were not able to obtain a reliable estimate of the cost per QALY threshold.
This result is unsurprising given the second key finding: cost-effectiveness evidence was very rarely used to justify expenditure plans, which were driven by a range of other factors including Scottish Government initiatives, patient convenience, political pressure and centrally-led waiting time targets.
Figure 1: Cost per QALY of marginal services in NHS Scotland 2012/13
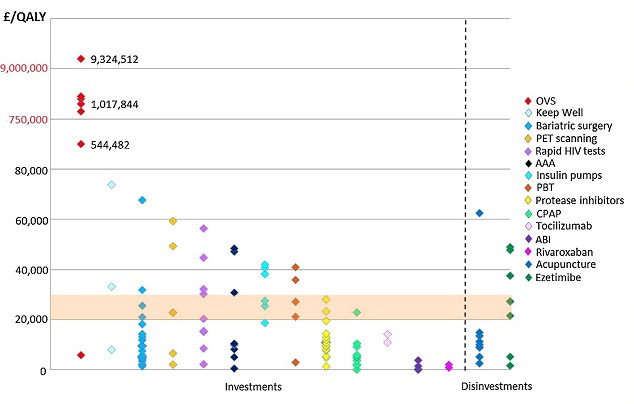
OVS = Orthoptic vision screening; PET = Positron emission tomography; AAA = Abdominal aortic aneurysm screening; PBT: Proton beam therapy; CPAP = Continuous positive airway pressure; ABI = Alcohol brief interventions
These results highlight the differences in objectives between HTA bodies (which make their recommendation decisions primarily on the basis of cost per QALY evidence) and local health service decision-makers. This has important implications for the interpretation of the threshold: if the NHS does not make spending decisions based on cost per QALY evidence, then a cost-effectiveness threshold expressed in QALYs is unlikely to represent the true opportunity cost of HTA decisions.
Finally, Sarah highlighted the difficulty experienced by the authors in attempting to locate evidence on the cost-effectiveness of various NHS services. She argued, therefore, that even if it were desirable, the use of cost-effectiveness evidence at local level would be highly challenging without extensive investment in health economics resources.
Sarah’s slides are available below:
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!